Table of Contents
ToggleUrinary incontinence is the involuntary leakage of urine and is a very common issue amongst women in the United States. Although urinary incontinence can occur at any time throughout the lifespan, women are more likely to experience incontinence after going through menopause.
Contrary to popular belief, having problems with urinary leakage is not a “normal” part of the aging process. Although some women have minor issues with incontinence and can tolerate wearing a pantiliner in case of leaks, others with more serious concerns may want to seek treatment for their incontinence.
If you find yourself skipping social events, avoiding long outings, or making sure you are always seated as close as possible to the bathroom, you may benefit from discussing treatments for incontinence with your healthcare provider.
This article will give you an overview of urinary incontinence, including:
- what kind of workup you might undergo
- what types of treatments are available for women with incontinence
Let’s start with a quick review of the way urination is supposed to work.
The Anatomy of the Urinary System
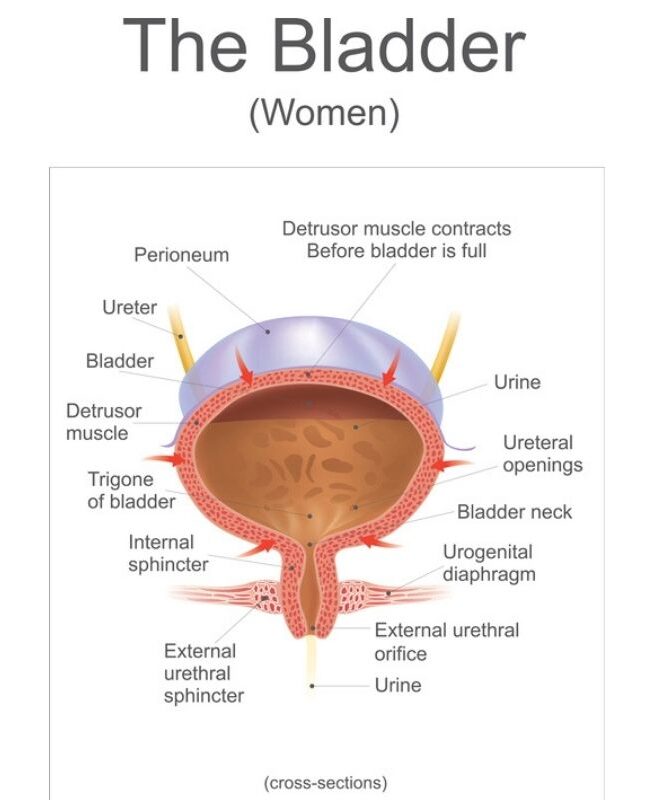
Urine is produced by the kidneys, flows through the ureters (long tubes connecting the kidneys and the bladder), then it is stored in the bladder. The bladder is made of muscle and is capable of stretching (similar to how the muscle of the uterus stretches during pregnancy), therefore allowing a large volume of urine to be stored before triggering the urge to urinate.
An average person can hold about 400-600mL in their bladder before needing to use the bathroom. The outlet of the bladder is known as the urethra. There are two sphincters (valves) which control the flow of urine out of the bladder. Your nervous system can sense the volume of the bladder and sends signals to your brain about the need to urinate.
You can ignore the need to urinate for a certain amount of time because the sphincters of the urethra don’t open without your brain’s “permission.” Once you are in the right place at the right time, your brain allows the sphincters to relax, the bladder muscles contract to empty out the urine, and you feel a sense of relief as the pressure in the bladder goes away.
There are multiple ways in which this normal chain of events can be disrupted and lead to incontinence. There are three main types of incontinence that women struggle with: stress incontinence, urge incontinence, and overflow incontinence.
Stress Urinary Incontinence (SUI)
Stress urinary incontinence, or SUI, refers to the leakage of urine upon applying additional stress to the bladder. For example, women with stress incontinence may leak urine whenever they cough, sneeze, run, or jump. Things that can contribute to the development of stress incontinence include a hypermobile urethra and intrinsic sphincter deficiency (ISD).
Urethral hypermobility occurs when the muscles of the pelvic floor are weakened and unable to keep the urethra closed during increases in pressure. Normally, with an increase in abdominal pressure (such as when you cough or sneeze), the pelvic muscles cause the urethra to remain closed so that urine does not spill out. When the pelvic floor muscles are weak, they no longer have the strength to keep the urethra closed against this increased pressure. Things that can cause the pelvic floor muscles to become weak include vaginal childbirth, chronic constipation, chronic cough (such as a smoker’s cough), and prolonged periods of heavy lifting (such as lifting heavy boxes for work). Obesity is also known to contribute to stress incontinence because the weight of the abdomen can cause increased pressure on the bladder.
Intrinsic sphincter deficiency (ISD) is less common than urethral hypermobility. This occurs when the urethral sphincter suffers a loss of muscle tone. Think of the sphincter like a rubber band which is tightly wrapped around the urethra. You can compare ISD to the rubber band being overstretched and worn out. It no longer has the tension needed to maintain a tight sealand prevent urine from leaking out.
Urge Urinary Incontinence (UUI)
Urge urinary incontinence (UUI) refers to the leakage of urine which is triggered by a strong urge to urinate. Some women may leak just a small amount while others might end up completely emptying their bladder. This can obviously make it very difficult to perform your daily responsibilities and to enjoy yourself when you are out with friends or family.
Many women experience urinary urgency but do not have the associated leakage. This can still cause significant disruptions to your daily life since you may be so uncomfortable trying to hold your bladder for prolonged periods of time that you find yourself avoiding certain activities or excusing yourself frequently to go to the bathroom.
UUI is caused by detrusor overactivity. The detrusor muscle is the muscle that contracts around the bladder in order to expel urine. When it is appropriate to urinate, the detrusor muscle should squeeze inwards, forcing the urine out through the urethra. After you have finished urinating, the detrusor muscle should relax and go back to its resting state, ready to give the signal when the bladder is full again.
When women suffer from urgency to urinate or UUI, it is because the detrusor is contracting when it shouldn’t be. This usually causes an uncomfortable sensation of bladder fullness, even if the bladder isn’t completely full. These contractions can be so strong that the urethral sphincter can no longer keep the urethra closed, which then leads to leakage of urine. There are some women who have symptoms of both SUI and UUI, this is referred to as mixed incontinence.
Overflow Incontinence
Women who experience constant leakage of urine, without a sense of urgency or additional stress on the bladder, are referred to as having overflow incontinence. Overflow incontinence can occur due to a weak, underactive detrusor muscle. This happens more commonly as women age, and can sometimes be a sign of a more serious underlying condition like diabetes or neurological dysfunction.
Another potential cause of overflow incontinence is an obstruction to the urethra known as bladder outlet obstruction. Things that can obstruct the urethra include large fibroids, pelvic organ prolapse, previous pelvic surgeries, and urethral strictures.
What to Expect at Your Appointment
When you schedule a visit with your healthcare provider to discuss urinary incontinence, you should be prepared to leave a urine sample at the start of the visit. An important first step in working up urinary problems is to ensure that there is no underlying urinary infection. Sometimes, women can have a urinary infection without realizing it. Treating an underlying infection can help reduce the frequency of incontinence episodes.
Your healthcare provider will have many questions about your urinary function. In addition to your full medical and surgical history, they will want to know how frequently you are having episodes of incontinence, whether you wake up in the middle of the night to urinate, if you have any burning or discomfort when urinating, and any tests or treatments you may have had in the past for your incontinence.
Your healthcare provider will also want to do a pelvic exam to assess the urethra, bladder, and vagina. It’s important to check for signs of pelvic organ prolapse, in which the bladder wall, uterus, or rectum can start to protrude into the vagina. Prolapse can contribute to urinary incontinence. Your healthcare provider will also check for signs of vaginal atrophy, or lack of blood flow to the vaginal tissue. This is a common issue in women who have gone through menopause and is due to a lack of estrogen in the vaginal tissues.
The vagina can appear pale and dry, and the skin of the vagina can be very fragile. This can make urinary tract infections more common and should be treated in women who are having urinary incontinence. Sometimes, the cause of incontinence can be obvious. In this case, your healthcare provider may choose to discuss treatments with you right away.
However, if they are having any doubt about what could be causing your incontinence or what the best treatment might be for you, they may recommend having further diagnostic studies done. There are two diagnostic studies which can be used when evaluating women with urinary incontinence: urodynamics testing and cystoscopy.
Urodynamics refers to several urinary studies that are conducted during an outpatient visit. These studies allow your healthcare provider to gain valuable insight into the way your bladder and urethra function. This information is helpful for deciding what types of treatments you could benefit from and for ruling out more serious causes of bladder dysfunction.
For women with mixed incontinence, it can provide a clearer picture of what is at the root of your symptoms. The test involves inserting one catheter into the urethra and one catheter into the vagina. Your healthcare provider may ask you to do a series of activities and to communicate the sensations you’re having during the tests. For most women, the catheter can be uncomfortable, but urodynamics is typically not a painful procedure.
Cystoscopy is when a camera is used to look inside of the bladder. This allows for a clear picture of the lining of the bladder and the openings to the ureters. This can help diagnose inflammatory conditions of the bladder as well as bladder masses which may be causing obstruction. This procedure is usually done in the office and typically causes only mild discomfort.
Talking to Your Healthcare Provider About Urinary Incontinence

Urinary incontinence is a common concern, but keep in mind it is not a “normal” part of the aging process. You don’t need to deal with the embarrassment and inconvenience that living with incontinence can cause. If you have any concerns with urinary incontinence, you should bring them up with your healthcare provider. There are a variety of treatments available for urinary incontinence.

Founder and Medical Director of ARIZONA GYNECOLOGY CONSULTANTS
Dr. Kelly Roy is a specialist in surgical gynecology and advanced laparoscopy (and hysteroscopy). She is a long-time resident of Arizona and obtained her Bachelor of Science degree in Biomedical Engineering at Arizona State University before finishing her Doctorate of Medicine at the University of Arizona in 1997.
Dr. Roy completed her residency in Obstetrics and Gynecology at the then “Banner Good Samaritan Hospital” (now Banner University Medical Center), in Phoenix Arizona in 2001.
Well known for her teaching and surgical ability, she is on the faculty at the residency program at both Banner University Medical Center and Saint Joseph’s Hospital in central Phoenix and is a Clinical Assistant Professor of Medicine at the University of Arizona College of Medicine, Phoenix Campus. Dr. Roy has taught advanced surgical techniques to medical students, residents, fellows and colleagues for over 15 years.
Dr. Roy is also a consultant to the medical device industry and has participated in the design and clinical testing of many instruments and surgical devices available on the world-wide market today.
Read More About Dr. Kelly Roy, MD | WebMD Profile | Health.USNews.com Profile | Current Obstetrics and Gynecology Reports: TFA with the Sonata System



