Table of Contents
ToggleMany women after having children, going through hysterectomy, or undergoing the aging process experience symptoms that are not only uncomfortable but embarrassing. There are products available that can help alleviate the humiliation, such as adhesive strip underwear pads, panties or disposable underwear. But those can be costly over time and put a damper on style and spontaneity. If you think you could be suffering from what is called a prolapsed bladder or cystocele, there are ways to help minimize the symptoms and possibly reverse the condition, noninvasively.
The Physical Attributes of Cystocele
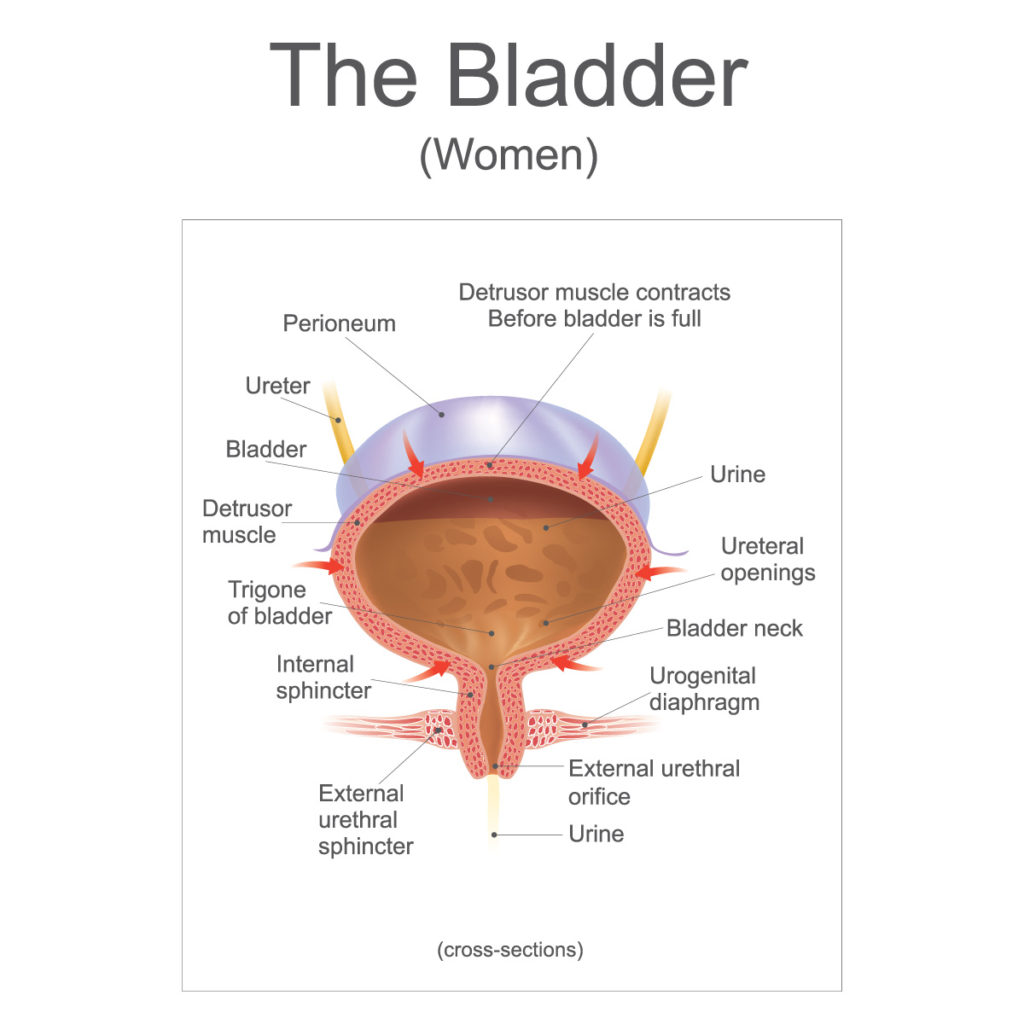
With cystocele it can feel as though your bladder is dropping. In a sense, it is. The bladder itself is a muscular-like organ, hollow, that resembles a balloon, expanding and retracting depending on the level of urine present. When a woman gets the urge to empty the bladder, urine flows from the bladder downward through the urethra and ultimately out of the body. The bladder is located in close proximity to other parts of the reproductive system, in the middle of both pelvic bones. Positioned alongside the urethra is the vagina, the connection point between the uterus and the outside. When prolapse happens, the bladder drops from its original position and protrudes into the vagina. As ominous as this may sound, many women who have the condition don’t know it.
Symptoms of a Prolapsed Bladder
There are many ways that the body provides an indication that a prolapsed bladder exists. Each woman is different and all symptoms don’t need to be met to have the condition.
Prolapsed Bladder Symptoms:
- Frequent urination
- Sensation of needing to urinate often
- Bladder leakage from pressure put on the area (or from coughing, sneezing, laughing)
- Partial voiding, when urine remains in the bladder
- Increase in bladder infections
- Pain in the lower back or pelvic area
- Feeling of heaviness, fullness, or droopiness in pelvic area
- Bladder coming through the vagina
- Difficulty when inserting vaginal applicators and tampons
After you’ve gone through the above list and identified which symptoms resonate with your day-to-day, find details below that indicate the various stages of prolapsed bladder.
Stages of a Prolapsed Bladder
Depending on how extensive the bladder has dropped, the options in how best to treat the condition will be discussed and a treatment protocol will be determined. A visit with your Ob/Gyn or other healthcare practitioner will uncover the specific stage of prolapse.
Prolapsed Bladder Staging
- Stage 1 – Mild condition, bladder has slightly extended into the vagina.
- Stage 2 – Moderate condition, bladder has dropped to the vagina opening.
- Stage 3 – Severe condition, bladder protrudes through the opening of the vagina.
Based on the type of symptoms, a doctor may want to insert a catheter through the urethra to measure how much urine is left in the bladder after voiding: this is termed postvoid residual. Other ways to examine the status of the bladder are through a bladder ultrasound using a transducer (creates sound waves for imaging) or an x-ray exam of the bladder, known as a cystourethrogram, that is done while a woman is urinating. The procedure does not require anesthesia though sedation is often an option.
If you are one of the many women experiencing any stage of bladder prolapse, it may come by you honestly.
Why Does the Female Bladder Drop Over Time?
Genetics do play a role in a woman’s predisposition to prolapsed bladder. In addition, hormones can also create the basis for its development. As we age, our natural levels of estrogen drop often compromising the vagina as estrogen strengthens the muscles that support it. Over time, the vagina weakens, and by the way of gravity, begins to fall. A repercussion to hysterectomy (partial and full) is the development of a prolapsed bladder. The National Institute of Health (NIH) studied the effects of hysterectomy on the female bladder and found a correlation. After these procedures, women will engage an immediate drop in estrogen production, which is often why some elect to include hormone therapy to their lives. However, this course of action may not circumvent the state of the bladder.
Other aspects of life may lead to a fallen bladder.
Prolapsed Bladder Causes
- Excessive coughing
- Physical activity that strains pelvic area
- Vaginal births
- Constipation and pushing through bowel movements
- Obesity*
*While obesity can predicate a fallen bladder, diet or specific nutrition is not directly linked to the condition.
Options in Treating Prolapsed Bladder
The stage of prolapsed bladder will often dictate the treatment choices available to the patient. The good news is that for many women, certain exercises will not only prevent prolapse but can do much to reverse the condition.
For women who have severe prolapse, surgery may be necessary to lift the bladder away from the vagina and reconstruct the vaginal wall to adequately support the bladder. A surgeon, usually a urologist or Ob/Gyn will tighten the tissue that surrounds these organs. The post-op for the surgery is between 4 to 6 weeks.
For moderate bladder prolapse, patients can be offered a vaginal pessary that is inserted into the vagina. The small device comes in a myriad of sizes to fit each woman as needed, keeping the bladder in place while providing the vaginal wall the support required, preventing further damage.
Exercise, will often be the panacea for women who are amidst early-stage bladder prolapse and also serves as a continual strength builder for the treatment and prevention of this condition. Here are some ways to add bladder health to your everyday regimen.
Kegel A Falling Bladder Back into Place
Strangely enough, there’s an exercise that can be done in the comfort of your car, your office or while sitting at the dinner table and no one will ever know you’re doing it. The exercise is called the kegel and it isn’t just for pregnancy. Men can find benefit from it too.
Meant to increase the strength of the vaginal wall and the ability to gain control over bladder control, kegeling can change your life for the better. The key to a proper kegel is to discern which pelvic muscles apply and to perform this exercise ritual faithfully up to 3 or 4 sessions a day for maximum benefit.
How to Kegel:
- Squeeze the genital muscles as if pulling them up from the inside.
- Each squeeze, should be able to (if desired) stop the flow of urine.
- Hold the squeeze for 3 full seconds.
- Release the squeeze.
- Repeat.
- Begin the exercise and complete 10 successions, to reach a total of 25 per day.
There is no reason to live with the discomfort and humiliation of a prolapsed bladder and its associated symptoms. Start kegeling. Seek a medical practitioner knowledgeable in this condition for a formal diagnosis and recommended treatment that will provide optimal results.

Founder and Medical Director of ARIZONA GYNECOLOGY CONSULTANTS
Dr. Kelly Roy is a specialist in surgical gynecology and advanced laparoscopy (and hysteroscopy). She is a long-time resident of Arizona and obtained her Bachelor of Science degree in Biomedical Engineering at Arizona State University before finishing her Doctorate of Medicine at the University of Arizona in 1997.
Dr. Roy completed her residency in Obstetrics and Gynecology at the then “Banner Good Samaritan Hospital” (now Banner University Medical Center), in Phoenix Arizona in 2001.
Well known for her teaching and surgical ability, she is on the faculty at the residency program at both Banner University Medical Center and Saint Joseph’s Hospital in central Phoenix and is a Clinical Assistant Professor of Medicine at the University of Arizona College of Medicine, Phoenix Campus. Dr. Roy has taught advanced surgical techniques to medical students, residents, fellows and colleagues for over 15 years.
Dr. Roy is also a consultant to the medical device industry and has participated in the design and clinical testing of many instruments and surgical devices available on the world-wide market today.
Read More About Dr. Kelly Roy, MD | WebMD Profile | Health.USNews.com Profile | Current Obstetrics and Gynecology Reports: TFA with the Sonata System

