Last month our very own Dr. Davitt was published in the Moon Valley Tattler, a local Phoenix East Valley news publication. The article, entitled “Don’t Let This Pain Make You Withdraw from Daily Life,” features a wealth of information about the one pain Dr. Davitt believes you don’t have to live with.
This pain is common in women, but that doesn’t mean you need to continue suffering. In fact, the longer women live with the pain, the more the pain can develop and become “worn in.” Worse, it becomes more difficult to treat. [1]Davitt, J. (2022, March 1). Moon Valley Tattler March 2022. Issue. Retrieved April 21, 2022, from https://issuu.com/moonvalleytattler/docs/moon-valley-tattler-march-digital Fortunately, there are easily accessible, minimally invasive surgeries and other techniques that can reduce this pain.
You Don’t Have to Live with Pelvic Pain
While pelvic pain is certainly common, it is not something you should have to go on living with. It’s vital that you share your symptoms with your doctor, so they can help you make an educated decision regarding what could be causing your pelvic pain and how to treat it effectively.

In the Moon Valley Tattler article, Dr. Davitt provided some key steps for finding pelvic pain relief:
- Schedule a consultation with an experienced doctor.
- Consider all treatment options, including minimally invasive surgery.
- Don’t suffer in silence – reach out to friends, family, and your doctor for support.
- Seek a second opinion if you’re not getting the results you want from your current treatment plan.
At Arizona Gynecology Consultants, we diagnose pelvic pain by listening to our patients and addressing their symptoms. These symptoms are important because there are multiple causes of pelvic pain, and to treat them, doctors must find the specific cause of your pain. Our doctors take the utmost care in making an in-depth diagnosis of your pain and treating it from the source

Pelvic Pain FAQ
Of course, pelvic pain can be debilitating to live with, even when you know there are many treatments available to help. To take the first step towards recovery from your pain, it’s important to learn more about what causes it. In addition, treatments vary depending on the symptoms you are experiencing.
Sometimes, women find their pelvic pain stems from a simple issue and the pain resolves completely with a relatively easy fix. In other situations, pelvic pain is chronic and requires long-term treatment to manage. Here are some frequently asked questions about pelvic pain to help you better understand this condition.
What Does Pelvic Pain Feel Like?
Pelvic pain can feel like an aching pressure radiating through the pelvic region, but it can also include sharper pains that contribute to extreme discomfort. This pain can happen anywhere below the navel in the lower torso region. Depending on the cause, pelvic pain can be constant, or it can come and go. It’s essential to watch for symptoms like lower back pain, unusual discharge, and bleeding. Pelvic pain can occur during or outside of a woman’s menstrual cycle, and you may experience discomfort during sexual intercourse. [2]U.S. National Library of Medicine (2021). Pelvic pain: Lower abdominal pain. MedlinePlus Resources. Retrieved April 21, 2022, from … Continue reading
How Do You Know If Pelvic Pain Is Serious?
There are a few key things to keep in mind that will help you determine if your pelvic pain is something you should worry about. If the pain is severe, constant, or getting worse over time, this may be a sign that you should relay your concerns to a doctor. As a rule of thumb, if your day-to-day life is impacted, you should see your doctor about your pelvic pain. You should also keep an eye out for other symptoms like fever, chills, nausea, and vomiting, as these could be signs of a larger problem.
What Are Some of the Causes of Pelvic Pain?
Pelvic pain can have a variety of causes, ranging from benign to serious.
Some common causes of pelvic pain include:
- Endometriosis. Endometriosis occurs when the lining of the uterus, called the endometrium, grows outside of the uterus.
- Ovulation. This occurs when an egg is ready for fertilization and released from the ovaries. It can cause cramping and even spotting outside of regular menstruation.
- Period cramps. A woman can experience spasming of the uterus during her monthly menstrual cycle.
- Pelvic inflammatory disease. This is an infection of the female reproductive system. It can damage organs and essential parts of the reproductive system as well as cause inflamed tissues in the area.
- Irritable bowel syndrome. When the bowels are irritated, they can cause abdominal pain and cramping.
- Kidney stones. When small pieces of calcium or other substances build up in the kidney, it leads to the formation of kidney stones, which can cause severe pain.
- Sexually transmitted infections. Sexually transmitted infections can be passed between sexual partners and can result in pelvic pain and other symptoms.
- Interstitial cystitis. This is a chronic bladder condition that can cause pelvic pain.
If you are experiencing pelvic pain, it is important to see a doctor so that the cause can be properly diagnosed and treated. Pelvic pain is not something you should have to live with, and there are many treatment options available.
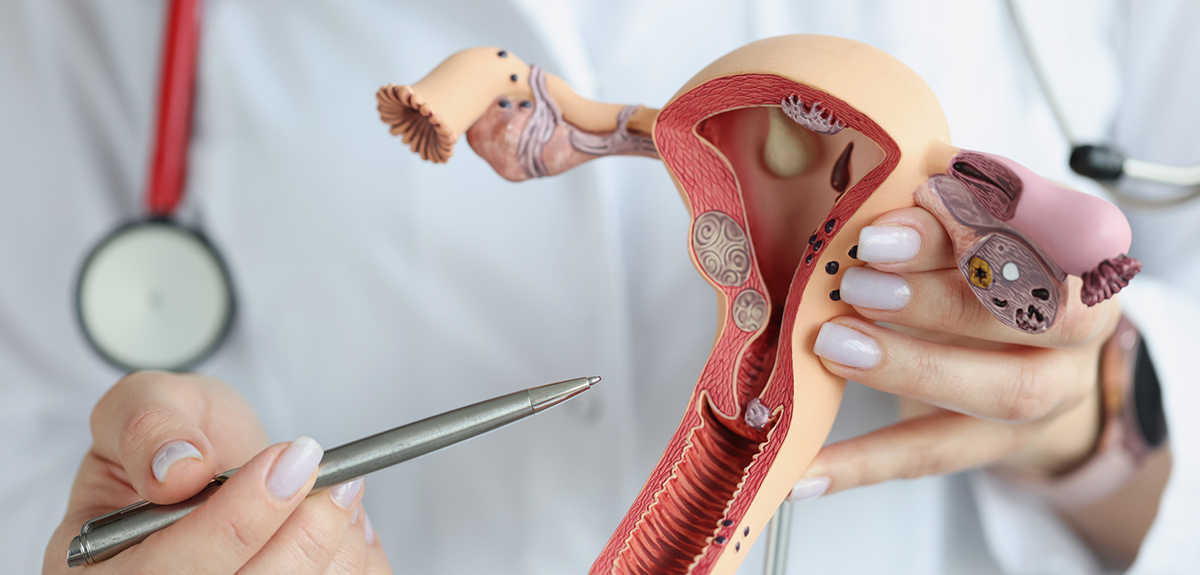
What Organs Are in My Pelvic Area?
A woman’s pelvic area is made up of the uterus, endometrium, fallopian tubes, cervix, vagina, and vulva. The uterus is the organ located in the lower torso of a woman, held between the bladder and the rectum. The uterus is responsible for receiving a fertilized egg and protecting a child if the woman becomes pregnant. The endometrium is the lining of the uterus, which thickens in preparation for pregnancy. If the woman does not become pregnant, this lining is shed each month during menstruation.
Women have two ovaries in their pelvis, which hold reproductive eggs. The fallopian tubes serve as a route for released eggs to travel from the ovaries to the uterus. The cervix is located at the lowest point of the uterus and serves as an access point to the outside of a woman’s body. The vagina is the canal that connects the external features of the reproductive system to the cervix, for the release and intake of fluids, birthing, and sexual intercourse. The vulva or vulvar region is the external part of a woman’s genitalia. [3]University of Rochester Medical Center (2022). Anatomy of the Female Pelvic Area. Health Encyclopedia – University of Rochester Medical Center (n.d.) Retrieved April 21, 2022, from … Continue reading
Why Does Pelvic Pain Get Worse at Night?
Pelvic pain often occurs as a chronic pain for many women. Chronic pain, in general, has been found to cause worse sleep at night and can keep patients awake. [4]Shaver, J. L., Iacovides, S. (2018). Sleep in women with chronic pain and autoimmune conditions: a narrative review. Sleep Medicine Clinics, 13(3), 375-394 … Continue reading While pelvic pain isn’t always worse at night, it may seem like it is, since you may notice this pain more as you are trying to fall asleep. People with chronic pelvic pain may suffer from insomnia due to this pain.
Does Lower Back Pain Cause Pelvic Pain?
Oftentimes, there is a neurological, orthopedic, or urological reason for back and pelvic pain. However, lower back pain doesn’t necessarily cause pelvic pain, but it can be a symptom of
pelvic pain. Lower back pain that is caused by pelvic pain can stem from adhesions in the uterus due to endometriosis. [5]King E. B. (1994). Back pain from the gynecological standpoint. California medicine, 68(2), 74–76. Retrieved April 21, 2022, from https://europepmc.org/article/med/7936502. It’s important to remember that pelvic pain can be a symptom of many different conditions. See a doctor to rule out any possible causes for your pelvic pain that may be leading to lower back pain. Your doctor must assess your pelvic region and any of the symptoms you have been having to determine if your back pain and pelvic pain are linked.
Can Bowel Problems Cause Pelvic Pain?
Irritable bowel syndrome (IBS) is a gut disorder that is diagnosed in many people. It mainly causes symptoms of bloating, diarrhea, and constipation, but it also commonly causes pelvic pain for women. IBS is often concurrent with chronic pelvic pain. IBS is even known to get worse during a woman’s menstrual cycle.
IBS tends to flare up and then remain dormant for periods of time. Although there isn’t a known way to fully cure IBS, there are ways to treat the condition. Treating your IBS could help address any pelvic pain you may be experiencing. It’s essential to work with your gynecologist to manage relevant symptoms and your gastroenterologist to assess your GI treatments.
How Can I Quickly Relieve Pelvic Pain?
There are a few things you can do to help relieve pelvic pain. First, try placing a heating pad on your lower abdomen or back. Heat often helps relax muscles and ease the pain. You can also try over-the-counter medications like ibuprofen or naproxen to help with pain and inflammation. If you find that you’re still in pain, consider scheduling an appointment with your gynecologist. They will be able to help you find the source of the pain and provide additional relief options.

What Are the 4 Pelvis Types?
As long ago as the 1930s, scientists identified four general pelvis types found in women. [6]Caldwell, W. E., & Moloy, H. C. (1938). Anatomical Variations in the Female Pelvis: Their Classification and Obstetrical Significance: (Section of Obstetrics and Gynecology). Proceedings of the … Continue reading These pelvis types are based on the shape and size of the upper area of the pelvis, or pelvic inlet. The pelvic inlet is where the birthing canal begins, before a baby must pass through the pelvic cavity in a woman’s body. These are the four types of pelvises:
-
Gynecoid
A gynecoid is the pelvic type most often found in females. The shape is very round, and it is a more open, shallow pelvis type.
-
Android
The android pelvis type is narrower and has more of a heart shape. It resembles a male pelvis because of its narrowness.
-
Anthropoid
The anthropoid pelvis has an oval or egg shape. It is known for being a narrower pelvis type with a bit more depth to it than other pelvis types.
-
Platypelloid
The platypelloid pelvis type is not very common and is often referred to as a flat pelvis. This pelvis type is very wide but doesn’t have a lot of depth to it.
While there are four basic types of pelvises, all women will have slightly different shapes and sizes, especially when it comes to the pelvic inlet. However, it is helpful to know the type of pelvis you have because it can help determine how easy or difficult it may be to give birth vaginally.
What Does a Pelvic X-Ray Show?
A pelvic X-ray can give a view of the bones in the pelvic and hip area for a doctor. Pelvic X-rays can help doctors identify tumors in the body, along with fractures, and any bone conditions a patient may have. If you have suffered an injury to the pelvic region, a pelvic X-ray can help show if there are any broken bones. A pelvic X-ray is also often used to diagnose the cause of pain in the lower abdomen or pelvis. This X-ray can help doctors see the bony structures in the pelvis and determine if they are the source of pain for a patient.
What’s the Difference Between the Hips and Pelvis?
The pelvis is made up of several bones that connect to form the pelvic girdle. The pelvis includes the hip bones, sacrum, and coccyx (tailbone). The hip bones are connected to the sacrum in the back and join in the front at the pubic symphysis.
In your hip joint, the head of the femur (thigh bone) sits in the acetabulum of the pelvis. The hip joint is what allows you to move your legs forward and backward, and from side to side. You can consider your hip bones as a component of your pelvis.
Can You Fracture Your Pelvis and Not Know It?
Typically, if your pelvis is fractured, you will know that it is fractured. It can cause severe pain when walking, and pain radiating through the pelvic and hip regions of the body. Pelvic fractures can also cause tingling and numbness in the area around your groin or in your legs. If you’re having a difficult time standing or urinating as well, you may want to have your pelvic area checked by an experienced doctor.
What Are Some Common Treatments for Pelvic Pain?
There are many different treatment options available for pelvic pain, and the best method will depend on the cause of the pain. Until you know the cause, try to avoid pushing yourself too hard through the pain. If your pelvic pain worsens while you are engaging in an activity, you should stop
Regardless of cause, some patients find enough relief with over-the-counter pain medications like aspirin, ibuprofen, or acetaminophen. Or, you can discuss with your doctor whether a prescription pain reliever is a good option for you. However, if your pain is chronic, pain-management medication alone likely will not solve the problem.
If the pain is due to a muscle strain or spasm, rest and ice may be enough to help relieve the pain. Your doctor may prescribe hormonal birth control or other medication to help ease pain caused by menstrual issues and other conditions. For example, if you have endometriosis, your pain may be addressed sufficiently with hormonal birth control. If you have pelvic inflammatory disease or other infection, your doctor will likely prescribe antibiotics to treat the infection before monitoring for residual pain.
In some cases, surgery may be necessary to remove scar tissue or vaginal cysts that are causing pain. For example, laparoscopic surgery can be used to remove adhesions or endometrial tissue via a tiny incision. If needed, a hysterectomy can even be performed laparoscopically or via the cervix. Your doctor will discuss the risks and benefits before recommending surgery.
Committed to Helping Those With Pelvic Pain?
Pelvic pain is very common, affecting more than one in every five women. However, it is not something that you have to live with. If you share your symptoms with your doctor they can work closely with you to identify the possible causes of your pain and provide effective treatment.

Kristina Calligan is a sub-specialty nurse practitioner in Women’s Health. A native to Arizona she obtained her Bachelor of Science in nursing in 2006 at Grand Canyon University in Glendale, Arizona. Never one to stop striving and achieving all that she could, she completed two master degrees in Nursing Science and Business Administration in 2012. Ms. Calligan joined Arizona Gynecology Consultants in 2009. Prior to working at Arizona Gynecology Consultants, she worked as a nurse in labor and delivery at several local hospitals and a research coordinator in women’s health care.
References
| ↑1 | Davitt, J. (2022, March 1). Moon Valley Tattler March 2022. Issue. Retrieved April 21, 2022, from https://issuu.com/moonvalleytattler/docs/moon-valley-tattler-march-digital |
|---|---|
| ↑2 | U.S. National Library of Medicine (2021). Pelvic pain: Lower abdominal pain. MedlinePlus Resources. Retrieved April 21, 2022, from https://medlineplus.gov/pelvicpain.html#:~:text=Pelvic%20pain%20occurs%20mostly%20in,way%20of%20your%20daily%20activities |
| ↑3 | University of Rochester Medical Center (2022). Anatomy of the Female Pelvic Area. Health Encyclopedia – University of Rochester Medical Center (n.d.) Retrieved April 21, 2022, from https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=p0054 |
| ↑4 | Shaver, J. L., Iacovides, S. (2018). Sleep in women with chronic pain and autoimmune conditions: a narrative review. Sleep Medicine Clinics, 13(3), 375-394 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1643162/?page=2 |
| ↑5 | King E. B. (1994). Back pain from the gynecological standpoint. California medicine, 68(2), 74–76. Retrieved April 21, 2022, from https://europepmc.org/article/med/7936502. |
| ↑6 | Caldwell, W. E., & Moloy, H. C. (1938). Anatomical Variations in the Female Pelvis: Their Classification and Obstetrical Significance: (Section of Obstetrics and Gynecology). Proceedings of the Royal Society of Medicine, 32(1), 1–30. Retrieved April 21, 2022, from https://www.researchgate.net/publication/280372450_Female_pelvic_shape_Distinct_types_or_nebulous_cloud/citation/download |


